The Baycrest Quick-Response Caregiver Tool was created to help caregivers/care partners respond to challenging behaviours expressed by persons living with dementia. The written material that follows is an explanation of the tool and how it is to be used. There are also 4 videos. There is a video called “Introduction” and 3 case scenarios involving actors. It is best to watch the “Introduction” video first. The 3 case scenarios involve a caregiver and a person living with dementia. In each situation, the caregiver tries to respond to a challenging situation using the Baycrest Quick-Response Caregiver Tool.
Baycrest Quick-Response Caregiver Tool TM Pocket Guide
It is strongly recommended that you download the pocket guide version of the Baycrest Quick-Response Caregiver Tool. This way you can refer to it quickly and easily when you need to use it. It can be printed out or you may consider saving it to your handheld device, tablet, or computer.
Download Here
Baycrest Quick-Response Caregiver Tool TM: Instruction Manual
Being a primary caregiver to a person living with dementia can present unique challenges. The person living with dementia may have changes in behaviour such as getting easily upset, wanting to leave, yelling, anger, and even physical behaviours such as pushing or hitting. These behaviours are not intentional, but rather a way that the person is trying communicate their needs or how they are feeling. Caregivers may feel overwhelmed and under-equipped to respond to these types of behaviours. To make matters more complicated, the person living with dementia will react based on how the caregiver responds to them causing behaviours to further intensify as illustrated in the following cycle:
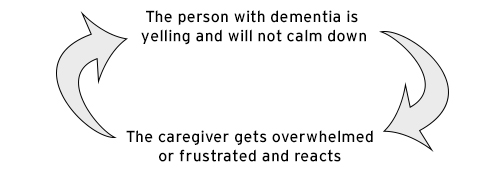
In this example of the cycle shown above, the person living with dementia is yelling and the caregiver does not know why. The caregiver becomes frustrated and irritated. This reaction by the caregiver causes more yelling and agitation in the person living with dementia, causing the cycle to continue.
The Baycrest Quick-Response Caregiver Tool tries to prevent this cycle from developing in the first place. The behaviour of the person living with dementia can be very difficult to understand – why is the person yelling? Is there some need that isn’t being met? Do they want something? Are they too hot? Are they too cold? Are they in pain? Are they scared? Are they bored? The person living with dementia may not be able to explain why they are upset and yelling.
The key is for the caregiver to not react immediately. That is where the Baycrest Quick-Response Caregiver Tool comes into action. By following a few steps, the caregiver may be able to better understand what is going on and address the situation more effectively.
Baycrest Quick-Response Caregiver Tool TM
The tool uses the acronym CARER to help remind caregivers of the 5 steps. Please see below:
C - (Step 1) Calm down (self-talk)
A - (Step 2) Attend to the interaction without immediately reacting
R - (Step 3) Reflect on your own feelings
E - (Step 4) Empathize with the other person’s feelings
R - (Step 5) Respond
Please click on the (+) sign below to see an explanation of each step.
-
Step 1: Calm down (self-talk)
We are all human and have feelings. We all react to situations and to other people’s feelings. The first step is to take a moment to try to calm down so that we avoid making the situation worse. Of course, this can be hard to do. The caregiver may step back, take some deep breaths, or use some positive self-talk to calm down and then do the next steps. Most of us can tell when we are getting angry or frustrated. The trick is to catch yourself right away and then step away.
-
Step 2: Attend to the interaction without immediately reacting
This step is meant to help the caregiver to remember that the person living with dementia is distressed. It is a matter of slowing down and taking a break before reacting to the person living with dementia. It is a time to remind oneself that the person living with dementia has an illness – their brain is not working properly and it is not their fault. The behaviours are not intentional. The person living with dementia may have a very hard time describing what they need. The caregiver must remember this: this person has a brain illness, is distressed, and can’t explain why.
-
Step 3: Reflect on your own feelings
Now that the caregiver has calmed down and has taken a short break to recall that the person has an illness that effects their brain, it is time for some self-talk. This is called “reflection.” The caregiver will ask himself or herself some questions:
- What am I feeling? (e.g., angry, frustrated, worried, sad)
- Why do I feel this way?
This is a very important step. Caregivers need to think about their own emotional reaction to what is going on. This involves reflecting on how one’s feelings and response can affect the person living with dementia. By trying to answer these two questions, the caregiver can begin to think through the situation and then consider how to best respond to the person living with dementia.
-
Step 4: Empathize with the other person’s feelings
Empathy is when someone tries to understand what the other person is feeling. Now it is time to consider what the person living with dementia is feeling. Some more self-talk:
- What is the other person feeling?
- Why is the other person feeling this way?
Now that the caregiver has become calm (step 1), remembered that the behaviours are unintentional symptoms of an illness (step 2), and considered his or her own feelings (step 3), and the feelings of the person living with dementia (step 4), the caregiver can now try to understand what the person living with dementia wants or needs and respond in a helpful, compassionate way.
-
Step 5: Respond
The caregiver can now try to understand what the person with dementia wants or needs and respond in a healthier and more helpful way.
Videos
Some examples of strategies to respond are outlined in the Supplementary Material. Please refer to the links below
Supplementary Material to Help Support Approaches to Managing Responsive Behaviours
Disclaimer: The tips provided are recommendations to help support responsive behaviour management. However, if behaviours persist, please consult with your care team for further guidance.
Special thanks to Dr. Yael Goldberg, Clinical Psychologist & Neuropsychologist, for the recommendations below.
-
Tips for Delivering Personal Care
- Use momentum: If you know that a person with dementia is resistive to personal care, set up a situation where you build momentum for saying yes to several tasks before introducing a task they typically say no to. That is, ask them to do a minimum of three things that you know they typically agree to, and then introduce the care task as item four. People are less likely to say no to something after they’ve been saying yes consistently.
- Identify the function of the behaviour: All behaviours serve a function. The four most common functions are:
- to gain attention
- to escape or avoid a task that is uncomfortable, unpleasant or aversive
- to gain access to an item (food/toy/activity)
- for self-stimulation (e.g., the behaviour itself feels good, or reduces some form of discomfort)
In the video, it appears that the function of the verbal aggression is to escape from personal care. And indeed, we see that it worked in that no care was provided. The person with dementia was verbally aggressive, and the staff left them alone. This just reinforces for the person with dementia that a good way to get out of personal care is to be verbally aggressive. The trick to unlearning this relationship between shouting and escape, is to provide the person with dementia with escape that is not contingent on their shouting. In practical terms, this means, offering frequent breaks and rewards for short intervals of participation in care activities. Over time, the person with dementia will learn to trust that they can get a break without the undesirable behaviour, and they will stop doing it altogether.
- Use simulated presence: To facilitate care, it may be helpful to play a video or audio recording of the person with dementia’s family member relaying a shared memory and asking the person with dementia to allow the staff to provide care. A script can be developed in advance, in collaboration with members of the health care team to maximize effect.
- Use familiarity: Familiarize yourself with the person with dementia’s preferences, likes, dislikes, and topics you can use to build rapport and trust. Consider preparing a person with dementia tip sheet/overview and keeping it somewhere accessible. This document would outline topics of conversation, interests and topics to avoid. Before entering the person with dementia’s room, staff can take a moment to review the tip sheet to assist with the interaction.
- Build rapport before care: Spend a few minutes chatting with the person with dementia to establish some familiarity and rapport. Building rapport, even routinely each day, can help increase cooperation with tasks, instructions and demands. Use topics from the list described above to talk about activities, events or topics of interest to the person with dementia.
- Present a “First/Then Contingency”: Consider presenting a “first/then” contingency, using something the person with dementia enjoys. In this scenario, if you know the person with dementia really enjoys coffee and cookies, after spending some time building rapport, you can then try to initiate care by letting her know what will come next, followed by something the person with dementia is known to enjoy (e.g., “OK, Mrs. P, I’m going to help you freshen up, and then I’ll get you a nice hot coffee with some cookies”). A first/then contingency has been demonstrated to increase cooperation with non-preferred tasks, if they’re followed by a preferred or pleasurable item or activity.
- Ask permission: Take a moment to ask permission before proceeding. Let the person with dementia know what you are going to do, count to 5 to allow them time to listen/respond and then proceed. Do this for each step of care you are going to provide.
- Let the person with dementia guide you: Wherever possible, do personal care at the time of day when the person with dementia is typically most cooperative. In the video, we saw that the person with dementia was woken up by the staff’s entry and turning on of overhead lights. She was confused and disoriented to person. A good strategy is to allow late risers to sleep in a bit later and let them wake up on their own so as not to be disruptive. Capitalizing on a person with dementia’s own natural rhythms will optimize successful outcomes.
- Choose your battles: If a person with dementia is distressed by changing clothes, under certain circumstances, you may wish to allow them to stay in the clothes they are in. For instance, if a person with dementia is resistant to putting on pajamas, you may wish to allow them to sleep in their clothes and then put on fresh ones the next morning.
- Use familiar staff: In the video, the person with dementia seems to be disoriented and does not recognize the staff. It is always a good idea to use staff that is familiar to the person with dementia.
- Consider trauma/reliving an abuse history: If a person with dementia has experienced trauma in the past, the provision of care may trigger re-experiencing. Sexual abuse trauma can particularly be confused with removal of clothing. The key is to provide reassurance and emotional support by telling the person with dementia each thing you are going to do before you do it. Try to use the same gender staff member where possible. Only uncover one body part at a time.
- Occupy the person with dementia’s hands: If a person with dementia is prone to become physically abusive, give them a small towel to hold to keep their hands busy.
- Play preferred music: Play preferred music during care to keep the person with dementia calm and relaxed. Sing with the music as you provide the care.
- Consider temperature: Make sure the room is warm, turn on a space heater if necessary. Heat the towel and/or wipes you will be using for care. Turn on the shower and get it warm before bringing the person with dementia in.
- Be ready: Prepare all care supplies, and lay everything out before you start care provision so that once you start, you can be efficient.
-
Tips for Using Re-Direction
Experiencing disorientation is very difficult for a person with dementia. As we saw in the video, a possible outcome of disorientation is intruding into areas that are not where the person with dementia belongs. Whether it be another person’s room, a locked linen cupboard or even the nursing station, intrusiveness can be very disruptive to others. It can be especially difficult to redirect a person with dementia who has a belief that you cannot disprove.
Here are some things you can try to help redirect person with dementias to other areas:
- Use redirection with a creative reason/rationale: Ask the person with dementia to come with you because you need to show them something in the hall, or because you need their help with something outside. Provide them with a purposeful task RELATED to what they’re currently doing. For example, you might say: “Oh wow you have done so much tidying! Come with me – let’s go get a laundry basket so you can fold and put away the rest of your clothes,” or “Let’s go put everything you’ve collected into the trash”.
- Use distraction: Once you have successfully used redirection and the person with dementia has followed you, utilize distraction. This could include talking to them about an entirely different topic while you’re walking, showing them something else of interest, leading them back to their room or another area, or engaging them in an entirely different activity to help pass their time (e.g., turning on the radio, bringing them to an activity, helping them to get seated in their room with a newspaper).
- Orient with something personally meaningful: To avoid similar situations in the future, consider placing personalized and familiar items, symbols, pictures, and signs on the entrance to the door of their room. This might include a bright name tag with their name on it, a large bright arrow pointing to their door, a picture of items/topics they enjoy (e.g., flowers, their family dog, a family photo, a photo of themselves). Remember, the items/pictures should be unique to the person with dementia, and you must consider their ability to see and recognize the various items placed in their environment.
- Avoid reality orientation: Do not try to convince the person with dementia that they are not in their own room. This will simply escalate conflict. Reality orientation will not result in increased cooperation and typically leads to more frustration.
- Use body language: Approach with a calm, friendly demeanour (e.g., shoulders relaxed, arms open).
- Use validation: Thank the person with dementia for completing the task they are currently engaged in (remember, in this scenario, the person with dementia thinks he is tidying his room, which is like a routine, long standing behaviour). Acknowledge what they are currently doing as a positive behaviour.
You might also try:
- Playing some music and dancing with them out of the room
- Inviting them out of the room to participate in an activity that they find personally meaningful (e.g., painting, ball toss, a concert)
- Telling them, “You’ll have time to tidy up your room later. Right now, it’s time for us to get ready for lunch,” and using the Gentle Persuasive Approach, gently guide them out of the room
-
Tips for Challenges in Giving Medication
Here are some strategies you can try when a person with dementia does not want to take their medication:
- Use the first/then approach: Find something (an object or an activity) that the person with dementia really likes, and offer it to them as a reward for engaging in the task. In this example, let’s say Mrs. Reilly really enjoys coffee and cookies. To apply the first/then approach, you would spend some time building rapport and then initiate medication administration by letting her know what will come next, followed by the thing she is known to enjoy. For instance, you could say “OK, Mrs. Reilly. First I’ll give you your medicine and then I’ll bring you a nice hot coffee with some cookies.” Be sure to offer verbal praise for agreement with the task. A first/then approach has been demonstrated to increase cooperation with non-preferred tasks, if they’re followed by a preferred or pleasurable item or activity.
- Offer choice: Give the person with dementia a sense of control and independence by offering them a choice. For instance, you might say, “Which pill do you want to take first?” Or “Would you like to sit here near the window or by your bed while taking your medication?” Or “Would you like to take your pills now or in 10 minutes?” Offer choice of beverages person with dementias can take the pill with (e.g., Would you like some juice or water? Apple or orange juice? Apple sauce or pudding?)
- Give a heads up: Inform the person with dementia of what is going to happen before it happens. For example, if medication is scheduled for 4pm, enter the person with dementia’s room at 3:45pm and inform them that you’ll be coming back in 15 minutes so they can take their medication.
- Consider preferences: Familiarize yourself with the person with dementia’s preferences, likes, dislikes, and topics you can use to build rapport and trust. Consider preparing and making this information available to all staff in the form of a person with dementia tip sheet/overview that can be kept somewhere accessible, outlining topics of conversation, interests, and topics to avoid. Take a moment to review this before you enter the person with dementia’s room.
- Build rapport before starting care: At eye level with the person with dementia, spend a few minutes chatting with the person with dementia to establish some familiarity and rapport. Building rapport, even routinely each day, can help increase cooperation with tasks, instructions, and demands. Use topics from the list described above to talk about activities, events or topics of interest to the person with dementia.
- Provide a written schedule: For person with dementias who are able to read and appreciate a schedule, create a schedule that outlines the activities of the day. Include things such as meal times, toileting, showers, recreational activities and medication times. Allow the person with dementia to hold on to the schedule, and refer to it as needed. Be consistent and make sure you stick to any schedule you provide. Make sure the written schedule is tailored for the person with dementia’s unique needs (e.g., large enough font, contrast, text that is clear, and written in their preferred or first language, and consider the use of pictures or images to illustrate the scheduled activities).
- Consult speech and language pathology: For some persons with dementias, there could be an underlying medical reason behind the refusal to take medication. For instance, as disease progresses, they may develop trouble swallowing whole pills which may go undetected by staff. It’s a good idea to rule this out by referral to a speech-language pathologist to do a swallowing assessment. If necessary, a recommendation may be to crush the pills and mix them in food such as jam, yogurt, pudding, or coffee. Sometimes spreading the jam over a piece of toast or a muffin can be very successful.
- Use familiar staff or a second person: It is always a good idea to use staff who are familiar to the person with dementia for optimal results. Consider having someone who is more familiar approach the person with dementia to take their medication. In this case, while the staff takes some time to regain familiarity with the person with dementia through increased contacts and building rapport, have a second person, who is familiar to the person with dementia, present at the time medication is given. Have this familiar person “re-introduce” the newer staff/person, to help build familiarity.
- Investigate contributing factors: The person with dementia’s misunderstanding of the staff person’s intent could be caused by a language barrier, psychosis, or simply cognitive decline caused by disease progression. It is a good idea to investigate these potential contributing factors to behaviour and consider alternatives such as translation cards, translation devices, picture communication tools, or visual supports.
Baycrest Quick-Response Caregiver Tool TM Pocket Guide
It is strongly recommended that you download the pocket guide version of the Baycrest Quick-Response Caregiver Tool TM. This way you refer to it quickly and easily when you need to use it. It can be printed out or you may consider saving it to you handheld device, tablet, or computer.
© 2019, Baycrest Centre for Geriatric Care. All rights reserved. A single copy of these materials may be reprinted/downloaded for non-commercial personal use only.